Prediabetes ICD-10: Why Is Coding Important for Prediabetes?

Prediabetes is a stage of abnormal blood rise just before diabetes. This condition is serious because many patients won’t know they’re close to slipping into full-blown diabetes until it’s almost too late. In fact, most people with high blood sugar diagnoses only get one after they’ve already developed diabetes. As has been proven over time, diabetes is difficult to reverse, so experts encourage people to treat prediabetes before it develops into high blood sugar.
There’s been a pressing focus on treating prediabetes since 2017, and the emphasis has become more relevant with lots of sensitization for Americans to create insurance for prediabetes. Since the tenth version of the ICD (International Code of Diagnostics) update, there’s even a specific principal diagnosis code for prediabetes. All of this highlights the importance of treating prediabetes before it worsens.
This guide highlights prediabetes, its code and identification with the World Health Organization (WHO), and the importance of the code to patients, providers, and insurers.
What to Expect
- What Is Prediabetes?
- The International Code of Diagnostics (ICD) and What It Means for Prediabetes
- The Specificity of the ICD-10 Code for Prediabetes?
- 2021 Prediabetes ICD-10-CM Diagnosis Code R73.03
- The History of the CODE R73.03
- Are There ICD-10 Codes Related to Prediabetes Code?
- Functions of the ICD-10 Code for Prediabetes in 2022
- Diabetes Prevention Programs (DPPs) and Their Role in Prediabetes Management
- Other Ways of Preventing Diabetes
What Is Prediabetes?
Prediabetes is a stage where high blood sugar is higher than normal but not so high that it can be diagnosed as diabetes. People with prediabetes are highly likely to be diagnosed with diabetes because the symptoms of the former aren’t so evident that people will be able to tell they need medical help.
Prediabetes has long been considered a part of the medical diagnostic-related group (DRG). For many experts, the condition is quite serious, meaning that patients will need to take it just as seriously as diabetes.
Recently, there have been many campaigns for patients to take routine blood sugar checks to know if they’re in the safe range. This is aimed to encourage healthy living among American adults. Health institutions believe early prediabetes diagnosis will help patients make much better decisions about their life and health.
Apart from the orientation of treating diabetes, the steady growth of prediabetes and the subsequent influx of diabetes has led to the World Health Organization (WHO) codifying prediabetes. Unlike the last nine versions of the WHO ICD classification, the 10th version has given prediabetes its specific code. The code was built to outline the importance of prediabetes awareness and treatment to improve the average American adult’s health.
The WHO classified prediabetes with its unique code so that patients’ providers and insurers can identify certain risk factors for the ailment and treat them with the same severity as other preventable mortality-threatening conditions. Following the classification, it’s become easier for patients to get insurance reimbursement, further diagnosis of prediabetes, and lasting treatment before they develop a worsened diabetes case.
The subsequent sections discuss prediabetes in terms of its relationship with the WHO ICD.
The International Code of Diagnostics (ICD) and What It Means for Prediabetes

The popular ICD is an abbreviation for the International Code of Diagnostics. It’s the World Health Organization’s international medical streamlining system.
The WHO started publishing diagnostic health issues with the ICD tag in 1948. The ICD version is updated over time; it’s currently in its 10th version, and it’s why all diagnostic conditions in recent times are termed ICD-10.
Virtually every country where WHO exists—over 100 countries—uses the ICD-10. As is well known, the United States is one of these countries and even provides funds to the medical organization.
The ICD-10 Is known to have more codes and specificity than the ICD-9 — its preceding version. While the ICD-9 has about 14,000 codes, the ICD-10 has over 70,000 codes (at least four times the former version).
For the ICD-9, prediabetes is classified as 790.29, representing “other abnormal glucose.” This means that prediabetes doesn’t have its specificity in the ICD-9. Rather, it shares the classification with conditions like steroid-induced hyperglycemia, hypoglycemia, and other 20 conditions and symptoms.
Currently, the ICD-10-M is the classification for mortality statistics. The ICD-10-CM means clinical modification (CM) for the 10th version of the International Code for Diagnostics (ICD).
The ICD-10-CM is typically used for prediabetes and its symptoms, also known as morbidities. The Center for Medicare and Medicaid (CMS) has published the categorization. For prediabetes specifically, the ICD-10-CM 73.03 is the coding specificity for the condition.
The Specificity of the ICD-10 Code for Prediabetes
The ICD-Code 10 generally deals with issues concerning high blood sugar and diabetes.
Below are some of the complications and their respective codes:
- The prediabetes ICD-10 code is R73.03
- The “R” in the Code for prediabetes is in line with the WHO Code section XVIII, which states, “Symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified”
- The “73” means “Elevated blood glucose level”
- The “.03” indicates “Prediabetes”
- “R70-79” implies “Abnormal findings on examination of blood, without a diagnosis”
2021 Prediabetes ICD-10-CM Diagnosis Code R73.03
The R73.03 in the ICD-10-CM code identifies prediabetes issues for reimbursement in 2021 concerning HIPAA-covered transactions. This code, however, isn’t to be used for an established diagnosis. This is because ICD-10-CM guards the code for the purposes already stated.
It can’t be used as a primary diagnosis code when there’s a definite diagnosis. “Latent diabetes” is also an inclusion term for this code as it’s considered prediabetes.
Some important facts about the ICD-10-CM R73.03 code are outlined below:
- The ICD-10-CM R73.03 2018 edition became effective on the 1st of October, 2017
- The ICD-10-CM R73.03 is the American coding identification for prediabetes; that of other countries can differ in terms of numbering
- The ICD-10-CM R73.03 covers latent diabetes conditions as well
As stated in this article, the R73.03 code isn’t the only code for diabetes-related conditions. Other codes come before it and are related to it in the listing, as we’ll see below:
- The R00-R99: This code highlights the “Symptoms, signs & abnormal clinical and laboratory findings, not elsewhere classified”
- The R70-R79: This code indicates “Abnormal findings during blood examination, without any definite diagnosis”
- The R73: This code simply indicates an “Elevated blood glucose level”
- The R73.0: This code identifies “Abnormal glucose”
All the above codes are above R73.03 and contribute to its formation. The ICD-10-CM R73.03 falls into the diagnostic-related group (category) (MS-DRG v35.0). Other diagnostic orders in the group include “640: Miscellaneous disorders of nutrition, metabolism, fluids and electrolytes with MCC.”
The History of the CODE R73.03
Claims of reimbursement with a service date on (or after) the 1st of October 2015 were mandated to use the ICD-10-CM codes.
Here’s an outline of how the code meaning has changed over time:
- 2017 (effective 10/1/2016) : New Code
- 2018 (effective 10/1/2017): No change
- Diagnosis Index entries containing back-references to R73.03
- Borderline diabetes mellitus R73.03
- Diabetes, diabetes mellitus (sugar) E11.9 latent R73.03
- Prediabetes, R73.03
Are There ICD-10 Codes Related to Prediabetes Code?
Certain ICD-10 codes are related to the prediabetes code ICD-10-CM R73.03. For a code related to prediabetes, they have to start with R73. This guide considers at least one of these in the codes that come before R73.03;
The R73, for example, indicates “Elevated blood sugar.” This doesn’t mean prediabetes.
Also, the R73.0, “Abnormal blood sugar,” stands for the consistent rise in body temperature but not prediabetes.
The R73.9 IS one code that’s significantly related to prediabetes. It indicates “Hyperglycemia.”
Some conditions that many people will expect to have related codes with R73.03 but don’t include:
- Types 1 & 2 diabetes
- Gestational diabetes
- Neonatal disorders
- Post-surgical hypoinsulinemia
- Hypoglycemia
All of these codes are grouped under ICD-10 as they’re considered diagnostic. However, they have different code patterns from prediabetes. Type 2 diabetes specifically is one that’s expected to have a related coding pattern to prediabetes since the latter often preceded the former, but the reverse is the case.
Functions of the ICD-10 Code for Prediabetes in 2022
The role of ICD-10 in prediabetes and other diabetes-related conditions is to create a unified understanding among all relevant stakeholders in the medical field. Classifying prediabetes with its ICD-10-CM R73.03 code allows health providers, insurers, and patients to stay on the same page regarding diagnosis and the relevant treatment and management they need to sort out the problem.
In the United States, any health body or organization that works with a healthy body will be able to understand precisely how the code works and what they can do concerning treatment, especially in the United States, where the code is incredibly relevant for communication.



Once a diagnostic has been classified as ICD-10-CM R73.03, it significantly reduces communication difficulty and payment requirements when an insurance firm is involved in some instances.
The below sections outline how important the code for prediabetes is in the United States for all respective groups of stakeholders:
Patients
The ICD-10-CM R73.03 is made known to patients after a diagnosis, and it’s what they’ll need to point out if they have to show it to a doctor or several doctors that didn’t exactly carry out the diagnosis themselves. Patients will also need the code when relaying their condition to an insurance company.
Providers
Providers use the code to pass information about prediabetes to patients and can use it as justification for more future diagnostic tests to understand its growth, reduction, and possible treatments.
Insurers
Insurers or insurance institutions use the code to implement patients’ financial reimbursements. In fact, one of the major advantages of the code is that it aids reimbursement approval for patients.
Statistical Significance
The ICD-10-CM code is also valuable for statistical purposes. Today, the United States has millions of people with diabetes-related conditions. The only way the WHO, the Centers for Disease Control and Prevention (CDC), and the American Diabetes Association (ADA) know these numbers so accurately is via the ICD-10-CM Code.
The National Center for Health Statistics (NCHS)—a body of the National Institutes of Health (NIH)—uses the ICD-10 data to trace and monitor population health. The institution uses the ICD-10CM R73.03 to know the number of people diagnosed with prediabetes annually. They can practically separate people with prediabetes from those with an abnormal rise in blood sugar or already in the diabetes stage.
The center uses the data revealed to tell if people with prediabetes are growing or if there’s been an impactful reduction following the sensitization and orientation carried out by ADA and other diabetes prevention programs (DPPs) in the country. It’s through the ICD-10-CM that the United States decided to allow reimbursement of DPPs after the steady surge of prediabetes annually for the past few years.
Diabetes Prevention Programs (DPPs) and Their Role in Prediabetes Management

The Diabetes Prevention Program (DPP) is one of the most effective campaigns the United States has come up with for people with prediabetes. DPPs are organized by public institutions like the CDC and a few private institutions.
DPPs are set up to help people with prediabetes reverse their blood sugar so they don’t develop diabetes. Several DPPs have succeeded in putting patients on the right track. Their primary approach is to help patients change their diet and live healthy lives.
More importantly, research has shown that patients admitted into DPPs have achieved higher success controlling and reversing their dangerously high blood sugar than those who attempt to do so themselves.
DPPs are incredibly helpful because patients are usually placed in a community of people with the same prediabetes issues. Together, they’re given personal assistants to help them achieve their goals and report their progress. So far, the result has shown that the campaigns have been incredibly effective.
Here are some of the major DPPs currently available:
CDC National Diabetes Prevention Program (CDC DPP)
The Centers for Disease Control and Prevention (CDC) has been at the forefront of handling prediabetes issues with its diabetes prevention program. The program, like others, is dependent on dieting and exercising.
Patients are taught and guided to get the best management treatment to enable them to reverse their condition and live healthier. Remarkably, the CDC DPP has achieved a lot of success in treating and reversing prediabetes.
YMCA’s Diabetes Prevention Program (YMCA DPP)
Although the YMCA isn’t as popular as the CDC, it’s just as effective in helping patients prevent diabetes by nipping prediabetes at the bud. The YMCA has helped men and women with the best management tips and professional health experts to treat their condition and live much healthier.
National Institute of Diabetes and Digestive and Kidney Diseases Diabetes Prevention Program (NIDDK DPP)
The NIDDK is another body committed to helping people with prediabetes treat their condition to live and lead a healthy life. Suffice it to say, the organization has helped people with top relevant treatments to handle their condition and reverse it.
Other Ways of Preventing Diabetes
While DPPs remains one of the most viable options, not every healthy person can afford to get registered. Thankfully, there are other ways that patients can treat and manage the condition.
The good thing is that the management method for prediabetes is similar to that of symptomatic diabetes. Below are some of the ways that people with prediabetes could manage their health:
Diet
DPPs are based on dieting. If people who can’t enlist in the program manager to control how much they eat, they’d have handled up to 50% of their troubles.
Medications aren’t recommended for prediabetes; on the other hand, natural methods like dieting are known to work wonders.
People with prediabetes must avoid foods filled with pure carbs, too much fat, or high sodium. The best foods to eat are those enriched with vitamins and minerals like magnesium and fiber. Several meal choices meet this criterion, and people who eat them can control their blood sugar better.
Exercising
Exercising is just as important as dieting. People with prediabetes can manage their condition better with proper eating and exercise.
Exercising with proper dieting burns off fats and reduces blood sugar drastically. It’s been proven to work many times, and it’s why many health institutions recommend exercising and cardiovascular activities alongside dieting.
Some of the best forms of exercise include running, brisk walking, jogging, swimming, and resistance training. Other more intensive forms include sprinting and high-intensity interval training (HIIT).
Intermittent Fasting
Intermittent fasting is often recommended for people who’re already diagnosed with diabetes or are keen on losing weight. However, prediabetes patients seeking to reduce their blood sugar faster can also opt for this method. The intermittent fasting method is reliable and consistently keeps to it, leading to fast weight reduction and better living.
Intermittent fasting simply means having a restricted time frame for eating. Once a person has an intermittent fast, they’re likely to eat only twice daily.
Some may start to eat for the day by 11 am and eat their last meal by 7 pm. During that time, they may only drink water and very low-carb juice. They may also eat a significantly light lunch.
According to many experts, the best restricted time window is the 16:8 window. This window means patients can only eat twice within 8 hours and not within the remaining 16 hours. People who eat by 11 am will have their last meal at a maximum of 7 pm, giving them enough time to sleep and rest.
Conclusion

Treating prediabetes is the best way to manage diabetes mellitus. Once a person develops prediabetes, they’re at a heightened risk of developing diabetes, a serious condition that can lead to death.
This guide considers prediabetes and the importance that health institutions now accord it such that it has its peculiar classification. As was revealed, the International Code of Diagnostics (ICD) for prediabetes is R73.03. This code is available in the tenth version of the ICD and has found use amongst patients’ health providers and insurers according to their ascribed limits.
The high level of attention towards prediabetes is rooted in how it’s become a serious concern over the years. Patients can now get insured for prediabetes treatment and apply practical management tips to manage the condition.
Dieting is one of the best management tips that people with prediabetes must take seriously. With dieting, people can quickly reverse prediabetes and live healthier lives. One of the best ways they can do so is to adhere to a diabetes-friendly diet through a diabetes management app.
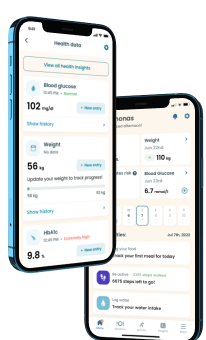
A diabetes management app helps people with diabetes and prediabetes regain blood sugar control. Our Klinio app is one of the trustworthy meal apps that people with prediabetes can trust at any time.
Our app provides prediabetes and diabetes patients with the best food to eat in terms of taste and blood sugar. This virtual caregiver also helps people with these conditions keep a good routine by providing them with a weekly and monthly plan for their meal choice.
Take a quiz and get your diabetes-management plan today!